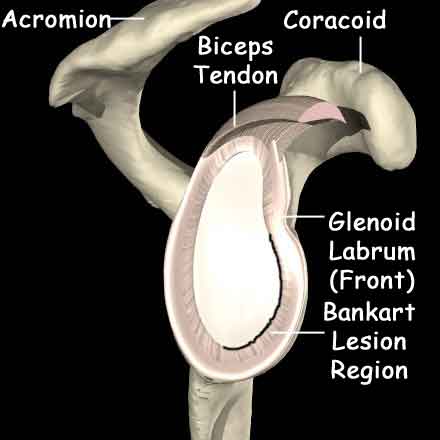
This is the most common form and usually occurs as a result of a fall in which the arm is twisted up and away from the body (as in preparing to throw a ball). The tissues at the front of the shoulder (the “labrum”) can be damaged, tearing them away from their attachment.
What are the signs and symptoms?
Acute dislocation causes severe pain in the arm which is commonly held by the side. Usually the patient is unwilling to allow anyone to touch the arm. Sometimes it is possible to see a swelling in the front of the shoulder.
How is the diagnosis made?
Acute dislocation is usually easy to diagnose based on the history and Xrays.
If the patient is seen at a later time (when the shoulder has been reduced) the history of the dislocation(s) will be taken and the shoulder examined. There are usually certain positions in which the shoulder feels as if it is going to dislocate.
Investigations include:
What is the initial treatment?
The first priority is to reduce the shoulder (put it back into the joint). Many people have been taught how to do this on the side of the pitch. If not then the patient will be requesting to be taken to hospital.
In hospital a combination of a painkiller and muscle relaxant is given and the shoulder manipulated back into the joint. The position will be checked with an X-Ray although the instant relief of pain is a good indication of success. Rarely it is not possible to put the shoulder back into the joint like this and a full anaesthetic is required.
The arm will be placed in a sling for 3 weeks followed by physiotherapy to strengthen the muscles.
If initial treatment doesn’t work, what’s next?
After a first dislocation there is a chance of dislocating the shoulder again with far less trauma because of the internal damage to the joint. The chance is higher if the patient is younger or is involved in contact sports. In some cases the chances can be as high as 80%.
If the shoulder keeps dislocating or if the patient is highly likely to suffer recurrent dislocation it may be necessary to operate to stabilize the shoulder.
Shoulder Stabilisation (Bankart repair)
On occasion the bone of the glenoid becomes damaged and a soft tissue repair is unlikely to work. If this is the case then the surgeon may recommend that the bone be rebuilt by moving a small adjacent bone – this is known as the Latarjet Procedure.